Lymphedema is a chronic condition that causes swelling in parts of the body, most commonly the arms or legs. It occurs when the lymphatic system, a network of vessels that drain fluid waste from tissues, is compromised. This can happen for various reasons, including damage to lymph nodes or vessels during surgery, radiation treatment, infection, or certain medical conditions. While there’s no cure for lymphedema, early diagnosis and proper management can significantly reduce swelling and improve quality of life.
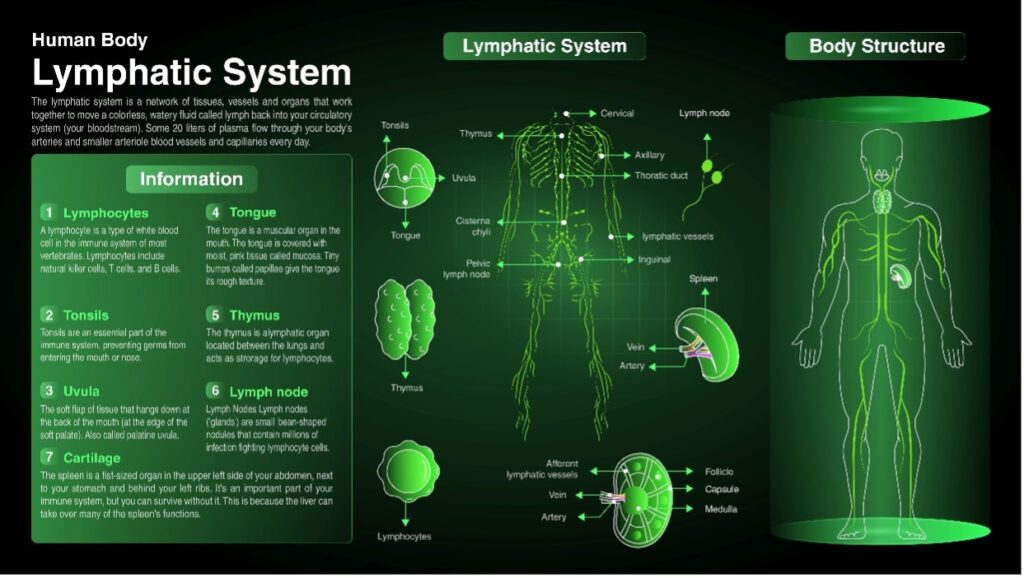
Understanding the Lymphatic System
The lymphatic system is a network of thin tubes and nodes that runs throughout the body, like the circulatory system but carrying fluid instead of blood. Lymph fluid collects waste products, toxins, and excess fluid from tissues and transports them to lymph nodes. Lymph nodes filter the fluid and fight infection.
Important Considerations
Lymphedema can affect any part of the body: While it most commonly affects the arms and legs, it can also occur in the head and neck.
Primary vs. Secondary Lymphedema: Primary lymphedema is caused by abnormalities in the lymphatic system present at birth, while secondary lymphedema develops due to external factors like surgery or infection.
Stages of Lymphedema: Lymphedema progresses through stages, presenting varying degrees of swelling. Early diagnosis allows for intervention before the condition worsens.
Knowing your risk factors is crucial for early detection. Understanding them can empower you to take preventive measures and ensure early diagnosis.

Risk Factors for Lymphedema
Several factors can increase your risk of developing lymphedema. Here’s a breakdown of the most common ones:
Cancer Treatment: Surgery, especially lymph node removal and radiation therapy, can damage lymph nodes and vessels, leading to lymphedema. The risk is higher depending on the location and extent of surgery or radiation treatment.
Liposuction: While uncommon, liposuction procedures, particularly those involving lymph node removal, can increase the risk of lymphedema.
Infection: Parasite infections like filariasis can damage the lymphatic system, leading to lymphedema, particularly in developing countries.
Obesity: Excessive weight gain can put pressure on the lymphatic system, hindering its proper functioning and increasing the risk of lymphedema.
Inherited Conditions: Milroy’s disease and Meige disease are rare inherited conditions that cause abnormal development of the lymphatic system, leading to lymphedema from birth (primary lymphedema) or later in life (secondary lymphedema).
Trauma: Injuries or burns that damage lymph nodes or vessels can increase the risk of lymphedema.
Deep Vein Thrombosis (DVT): Blood clots in the deep veins can impede lymphatic drainage, potentially leading to lymphedema.
Signs and Symptoms of Lymphedema
Here’s the most common:
Swelling in an arm or leg, sometimes accompanied by a feeling of heaviness or tightness.
Pitting edema: Pressing the swollen area leaves an indentation that persists for a few seconds
Skin changes: Thickening or hardening of skin, discoloration, or development of blisters or warts.
Reduced range of motion: Difficulty moving the affected limb due to swelling and stiffness
Discomfort or pain: Aching or throbbing pain in the swollen area.
If you experience any of these symptoms, especially after undergoing cancer treatment, surgery, or experiencing trauma, consult your doctor immediately. Early diagnosis and intervention can significantly improve the outcome.

What to Do if You Think You Might Have Lymphedema
If you suspect you have lymphedema, it is crucial to contact your doctor or certified lymphatic therapist. Early detection and treatment can help avoid complications and enhance your quality of life. So, if you notice any signs or symptoms of lymphedema, don’t delay seeking medical attention.
Treatment Options for Lymphedema
There is no cure for lymphedema, but there are treatments that can help manage the swelling and discomfort. Here are some of the most common treatment options:
Manual lymphatic drainage (MLD): A specialized massage technique that encourages fluid drainage from the affected area. A professional and certified lymphatic massage therapist does this. Theresa Gamlin from San Diego, CA, is a certified lymphatic massage therapist who has helped many people in southern California find relief. Read more about her services from the Orange Digital Technologies article here.
Compression garments: Elastic sleeves or stockings that help to reduce swelling and prevent further fluid buildup.
Skincare: Maintaining good skin hygiene and moisturizing regularly can help prevent infections.
Exercise: Regular exercise can improve circulation and lymphatic drainage.
Pneumatic compression therapy: A pump device that inflates and deflates sleeves or wraps to promote fluid movement.
In some cases, surgery may be an option to reduce swelling or improve lymphatic drainage.
Disclaimer: This blog post is intended for informational purposes only and should not be taken as medical advice. Please consult with a qualified healthcare professional for any questions or concerns regarding lymphedema.
More Information and Sources: